Beware of what reacts with your drugs. What might be good for people who haven’t had a transplant might not be good for recipients. Check with your doctor before commencing any new medication.
Drug
Whether you are prescribed a short-term course of medicines (i.e. antibiotics) or are treated for another chronic condition (long-term therapy), be aware of interactions with your anti-rejection  medications. For example, there are many drugs that may cause the cyclosporin or tacrolimus level in the body to change significantly.
medications. For example, there are many drugs that may cause the cyclosporin or tacrolimus level in the body to change significantly.
Some antibiotics such as erythromycin, roxithromycin, fluconazole can lower the amount of anti-rejection drug in the body causing a high risk of rejection, whilst drugs such as rifampicin, St John’s Wort and phenytoin can cause high levels of drug to remain in the body, increasing the risk of toxic side effects.
Food
 Check with your pharmacist to determine foods that you need to avoid or restrict whilst taking transplant medication, as they may interact. A common fruit for recipients to avoid is grapefruit and products containing grapefruit.
Check with your pharmacist to determine foods that you need to avoid or restrict whilst taking transplant medication, as they may interact. A common fruit for recipients to avoid is grapefruit and products containing grapefruit.
Chemicals present in grapefruit can affect the way transplant medications are absorbed in the body. If you’re taking tacrolimus, grapefruit can increase the tacrolimus levels in your body leading to potentially dangerous side effects.
Superfoods like goji berry, spirulina and kale have not been tested as yet for interaction with transplant medication and must be consumed with caution.
For more on eating to keep your transplant safe, check out our transplant-friendly recipes.
Herbal remedies
There are many herbal supplements available, often marketed as cures for illnesses. While some herbal medicines can be harmless and possibly helpful, there are others that can pose a serious health risk or interact with anti-rejection medications.
Abnormalities in liver function tests have been reported after use of certain herbal preparations, and there have been a number of rejection episodes reported in liver transplant patients using St John’s Wort, which people take for depression. These herbal preparations may interact with the absorption or metabolism of your anti-rejection drugs, making them less effective in the long run.
In general, it is best to avoid herbal remedies unless you have specific clearance from your transplant doctor.



 When you swallow a medicine, it gets absorbed by the body and the amount absorbed depends on whether your stomach is full or empty. Therefore certain medicines should not be taken with food. The food in your stomach can delay or decrease the amount of drug that is assimilated in your blood. If the amount of anti-rejection medicine absorbed is less than expected, there is a risk of organ rejection.
When you swallow a medicine, it gets absorbed by the body and the amount absorbed depends on whether your stomach is full or empty. Therefore certain medicines should not be taken with food. The food in your stomach can delay or decrease the amount of drug that is assimilated in your blood. If the amount of anti-rejection medicine absorbed is less than expected, there is a risk of organ rejection. Some medicines need to be taken with food to work better and cause less side effects, e.g. it is recommended to take prednisone with food. On an empty stomach, the drug may irritate the stomach lining and cause stomach upsets.
Some medicines need to be taken with food to work better and cause less side effects, e.g. it is recommended to take prednisone with food. On an empty stomach, the drug may irritate the stomach lining and cause stomach upsets.
 Hunger cravings and weight gain
Hunger cravings and weight gain
 V
V Muscle cramps
Muscle cramps Stomach irritation
Stomach irritation
 Trembling or shaking. You might notice this impact the most a few hours after taking some medicines when the concentration of the drug peaks in your blood. Things like gripping small things or writing can be tricky, but does not affect mobility and only minimally impacts everyday life.
Trembling or shaking. You might notice this impact the most a few hours after taking some medicines when the concentration of the drug peaks in your blood. Things like gripping small things or writing can be tricky, but does not affect mobility and only minimally impacts everyday life. Insomnia
Insomnia Increased hair growth/hair loss
Increased hair growth/hair loss Headaches
Headaches
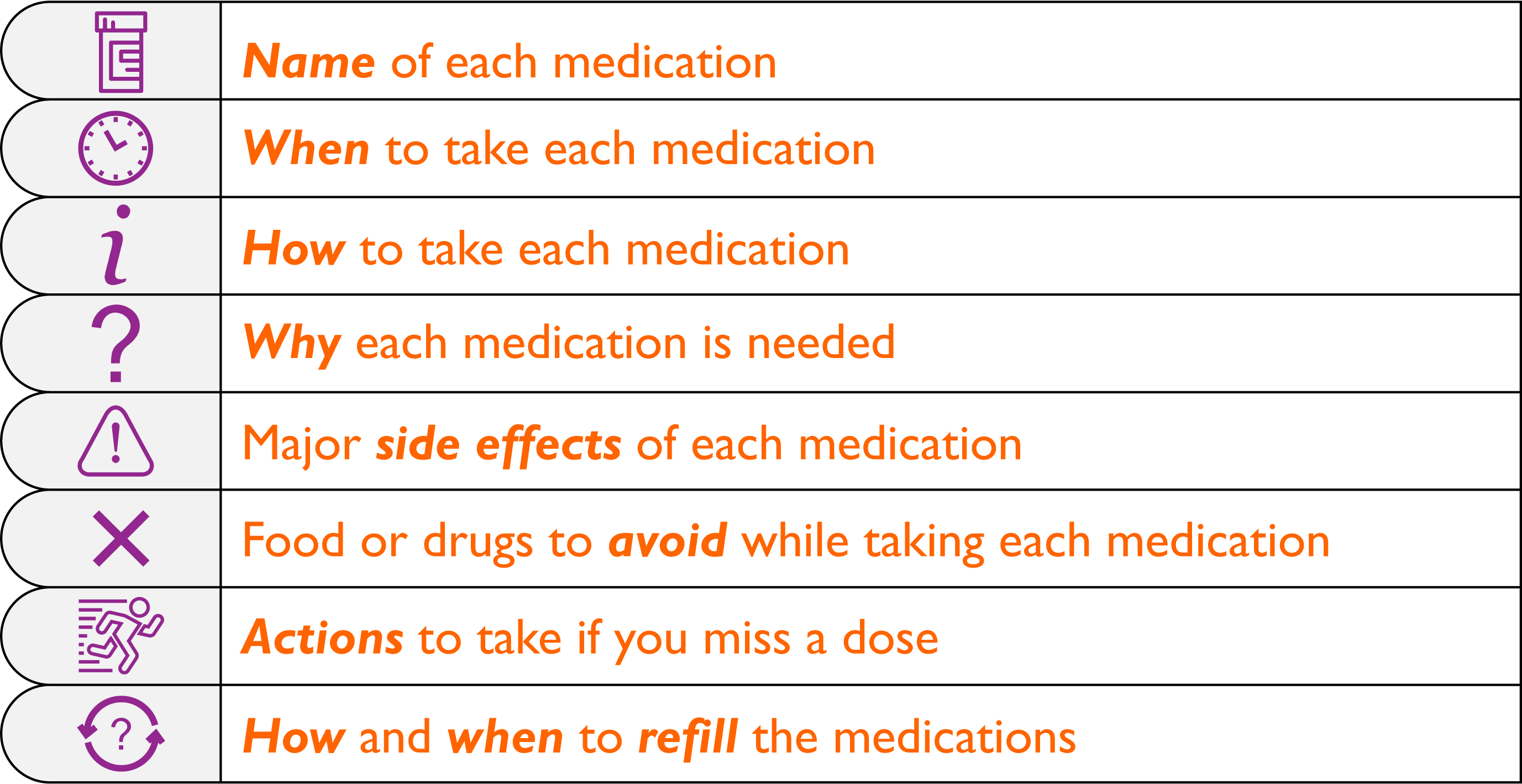
 In a complex medication regimen for an organ transplant it is recommended that you
In a complex medication regimen for an organ transplant it is recommended that you 
 medications. For example, there are many drugs that may cause the cyclosporin or tacrolimus level in the body to change significantly.
medications. For example, there are many drugs that may cause the cyclosporin or tacrolimus level in the body to change significantly. Check with your pharmacist to determine foods that you need to avoid or restrict whilst taking transplant medication, as they may interact. A common fruit for recipients to avoid is grapefruit and products containing grapefruit.
Check with your pharmacist to determine foods that you need to avoid or restrict whilst taking transplant medication, as they may interact. A common fruit for recipients to avoid is grapefruit and products containing grapefruit.
Recent Comments